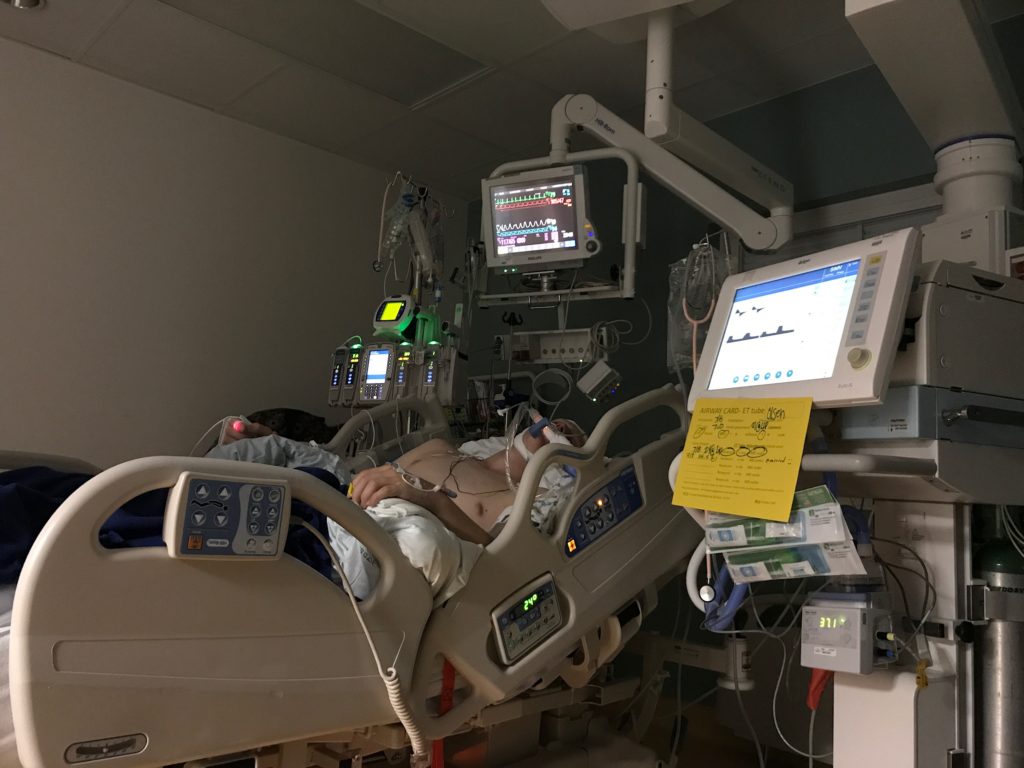
The Acute Phase: Holding Our Breath
The Social Worker at Primary Children’s Hospital told us that writing in a journal can be therapeutic. Even more, perhaps sharing our journey these past few weeks may help other families with children who suffer from this rare, devastating disease.
ICU Day #29 (Friday, July 28th)
9:00 AM: While Drew was in Radiology yesterday, they moved him to a new room in the ICU. The nurses and doctors know we are looking at another 10 to 14 days here in the ICU, so they moved us to the ICU room with the most windows, hoping it might help to cheer us up. Also, they wanted to move him to a room that had been thoroughly cleaned from any C-Diff or other germs since Drew will be immunosuppressed the next little while with the plasmapheresis treatments. We have now been in five rooms in the ICU: 2313, 2303, 2321, 2305, and 2314.
Drew continued running a fever last night between 38.8 and 39.4, but the nurses put a cooling blanket under him and turned the thermostat down in his room to 65 degrees, and this morning his temperature is under 38.0. I had to wear a jacket and get two blankets from the nurses so that as I spent the night in his room, I wouldn’t wake up with hypothermia.
4:00 PM: First round of plasmapheresis today starting about 1:00 this afternoon and lasting about 2 hours. The doctors also decided that it would not make sense to give Drew IVig after each plasmapheresis treatment only to have it wash out in 2 days. Instead, they plan to replace his plasma with donated plasma because it has most other parts of immune system to fight infection anyway. Then after the 5th plasmapheresis treatment, they will give him the IVig as it is longer lasting in his system.
8:30 PM: Somebody suggested that Dawn and I go out on a date or something and take some time away from the hospital. I had to chuckle. Even though I appreciated the sentiment, there is no way I could concentrate on anything else right now. Alex has vowed not to watch the new Spider Man movie until he can watch it with Drew. Some of Dawn’s family were at Lagoon (a local amusement park) today, and they invited us to go, but we would have just worried sick the whole time and wished we were by Drew’s side. I did ask Dawn to make sure she agreed, and she did.
ICU Day #30 (Saturday, July 29th)
10:00 AM: Pretty quiet last night. His tummy still a little distended. They also gave him some Lasix to diurese some fluids off. No fever. Lungs clear. The nurses noticed at some time between 2:00 and 2:30 this morning that his EEG was showing no bursts at all. So the doctors backed his Pentobarbital drip down from 6 to 5. We finally saw a burst about 8:00 this morning, and he is having a burst every 2 or 3 screens. When the doctors rounded a short time later, they backed his sedation down from 5 to 4. Just hoping for a quiet day with no fevers and no infections.
3:00 PM: Our ward Relief Society came to the hospital today to prepare the McDonald’s Room lunch for families in of hospital patients. In all, about 9 adults and 2 of their children came and helped cook, serve, and clean up an awesome potato bar with all the fixin’s. A lot of people have asked how they can help, and since we are limited with visitors and anywhere to store items at the hospital, some of our Relief Society from our church decided they would donate a meal to serve at the McDonald’s Room (they called themselves “Team DREW”) and not only bless our family, but also many other families in the hospital. They didn’t know it, but Dawn sat and cried while she ate her lunch because of how overwhelmed she was by their love and support. We were extremely grateful to spend time with friends and neighbors and have a delicious meal and service on behalf of Drew.
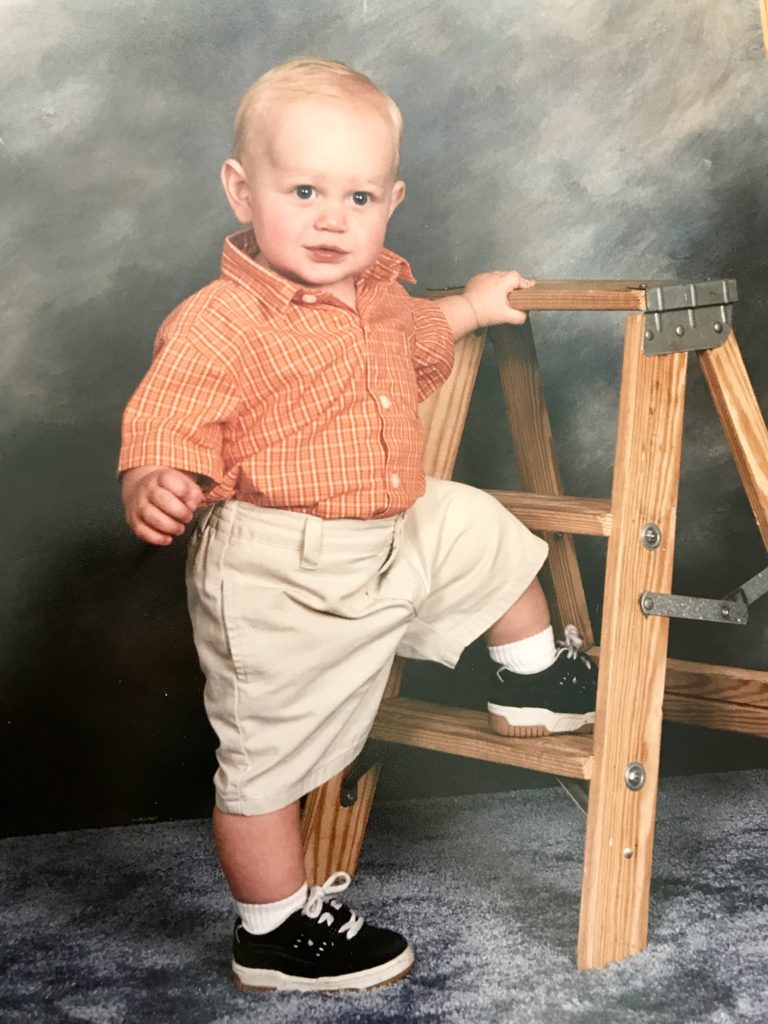
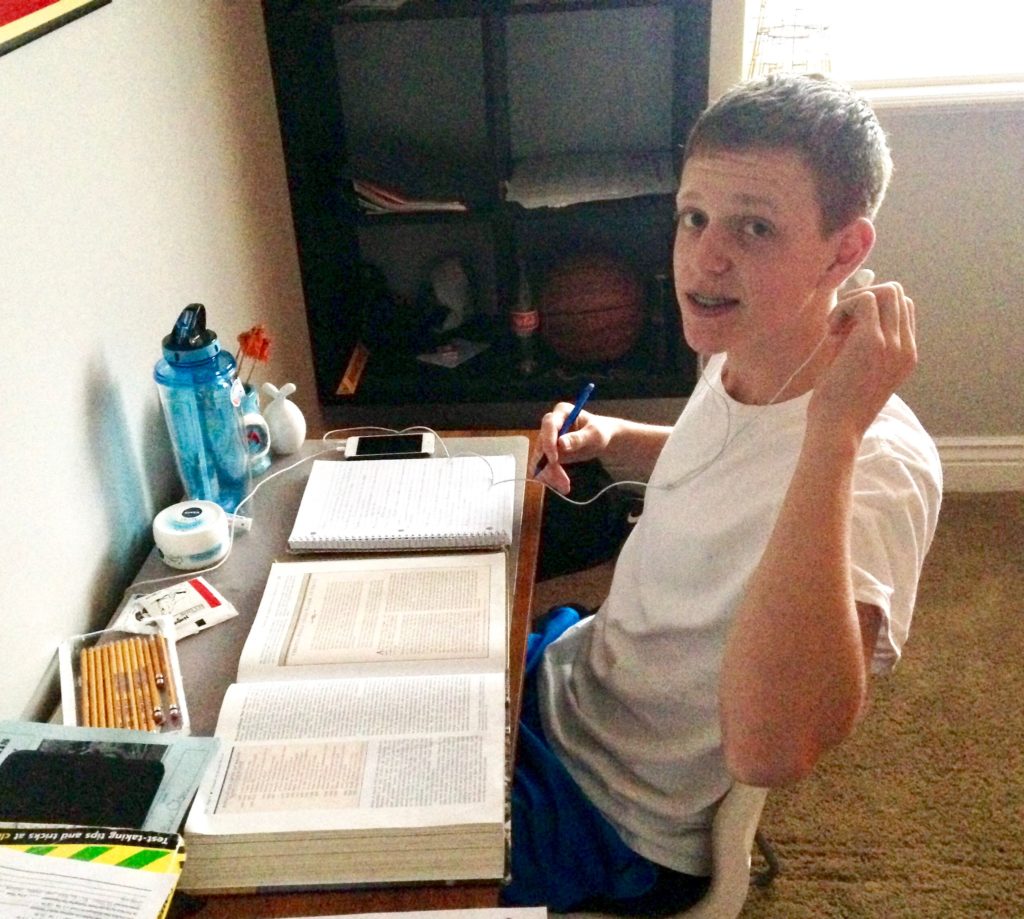
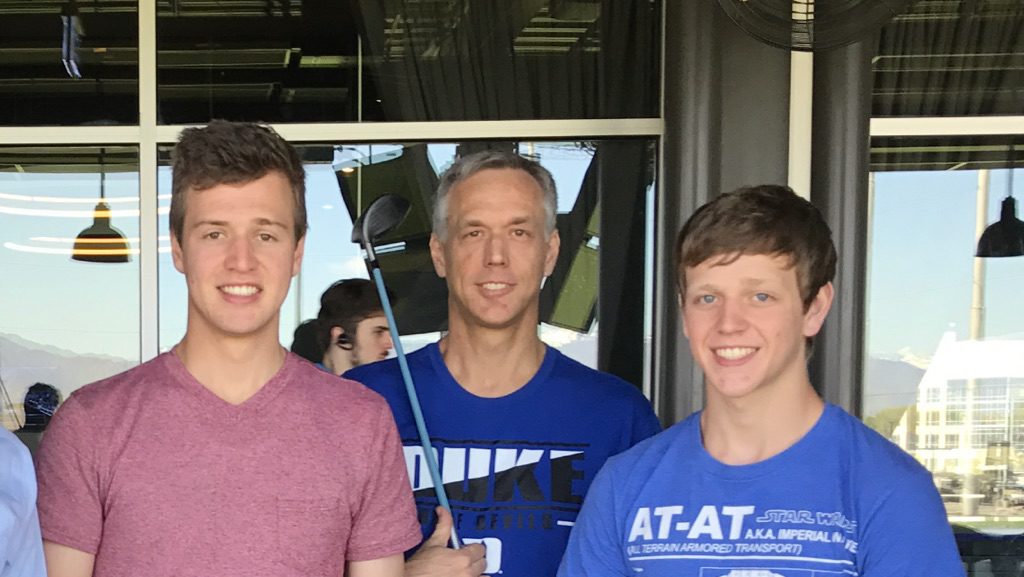
7:00 PM: Our family spent the afternoon swapping pictures and videos of Drew that we each had on our phones. We were really missing him today. I think part of it may have been seeing pictures of his Boy Scout troop return from their summer campout this afternoon. Knowing that Drew should have been camping and hiking with the past few days instead of lying in a medically induced coma was pretty hard. Plus the fact that he has been in the ICU for essentially a month now, and unconscious for more than 3 weeks, we are all getting more and more anxious and nervous, hoping that these plasmapheresis treatments will work this next week. We cried and laughed at some of the memories we had with Drew from the past few months, and made us more than ever pray to get him back.
ICU Day #31 (Sunday, July 30th)
8:00 AM: A relatively quiet night. No infections. No fever. Labs have been good. They did give him some extra laxatives and medication to help his bowels get going. They also planned to increase his Lasix to remove some excess fluid from his lungs and abdomen. They also asked Respiratory therapy to be more aggressive with his breathing treatments and suctioning every 4 hours.
7:30 PM: Drew received his second plasmapheresis treatment today from about 11 AM to 1 PM. Everything went well with the plasma, but they are going to hold off giving him a Pentobarbital bolus this time and just keep his sedation dose at 4 for now and just see if he needs adjustment later today.
9:00 PM: Alex and Ashley and I went to church at home today, and I was scheduled to teach a lesson to the Young Men and Young Women combined. I was fortunate to have one of the bishopric counselors also teach part of the lesson, and then I taught at the end. I really wanted to stress with the youth that people are more important than things. We read some stories from the scriptures, and then I talked about being nice to your family and those around you, because you never know when they may be taken from you. This evening we spent time visiting with several friends, neighbors, and family members as many loved ones stop by on Sunday afternoons and evenings to get updates and give love and support.
ICU Day #32 (Monday, July 31st)
3:30 AM: I used to like to sleep, but not so much any more because now when I sleep, I have bad dreams. The longer Drew has been unconscious, the worse the dreams have been getting. Well, I just had a really bad dream. Next to Drew’s bed every night I sleep in a recliner that is positioned so I can just open my eyes and see him and his monitors. I was kind of in that half-awake, half-asleep state, which might be why it seemed so real, but I thought I opened my eyes and saw Drew wide awake, sitting up in his bed, trying to scream but he couldn’t because of the breathing tube in his mouth. His eyes were wide open and looking right at me. I sat bolt upright in the recliner, my heart pounding out of my chest, and then I realized I had been dreaming. He still lay there in his medically induced coma, but I was wide awake and I cried for a while. I hate sleeping.
7:30 PM: They took him off his feeds and are just giving him IV fluids till he can have a bowel movement. They are doing another enema right now. His stomach is really swollen and tight, so we hope things get moving soon. Today is one of the in-between days while we wait for the next round of plasmapheresis.
When you have a loved one in the ICU, your schedule becomes dictated by everything going on around you. The doctors do their rounds at specified times. The medications are on a schedule. There is time dedicated to bed baths and repositioning and respiratory treatments. The same can be said about watching people as you sit in the lobby and I am reminded of the ocean tides as people ebb and flow, in and out of the hospital.
ICU Day #33 (Tuesday, August 1st)
4:30 AM: Drew just received his second chest X-ray of the night. The nurse noticed Drew’s breathing tube had started to become a little loose, so he asked the respiratory therapists to come secure it. They worked on it for quite a while around midnight, but finally got it. However, about an hour later, Drew’s oxygen dropped into the 80’s and the nurse noticed his left lung was not inflating as much as the right side. So they took the first chest X-ray to see if the breathing tube needed to be adjusted, but it was fine. The nurses turned Drew to his other side to see if that would help, and after a couple of hours his left lung seemed to be inflating better, but his oxygen was still a little lower than it had been, which was why the doctor ordered a second chest X-ray. I got to look at it over the nurse’s shoulder, and although the breathing tube looked fine, his lungs look milky, just like they did when he had pneumonia a couple of weeks ago.
10:30 AM: The doctors stop by on rounds. The third round of plasmapheresis is scheduled to start in a half hour. He had a small bowel movement yesterday, but not nearly enough to allow them to re-start his feeding tube, so they plan to try more aggressive treatments today to help get his intestines moving again. Lastly, they confirmed that Drew does have pneumonia again, which we were disappointed to hear, but not unsurprising as he has become immunosuppresssed. They plan to start antibiotics immediately to stay on top of the pneumonia while they wait for the cultures to come back.
In the 2000 movie, Cast Away, Tom Hanks plays Chuck Noland, a FedEx executive, who survives a plane crash and becomes stranded on a deserted island. For some reason this movie popped into my mind as Tom Hank’s character tries to survive day after day the mental, physical, and emotional strain of survival. After four years on the island, some trash washes up on the shore one day that he is able to use to construct a sail for a raft, and (spoiler alert) he is ultimately able to be rescued by a passing ship and he returns home to Memphis, Tennessee.
I guess in a way, the uncertainty of Drew’s eventual recovery has brought every gamut of mental, physical, and emotional strain, just like Tom Hank’s character felt as he waited on the island for something to wash ashore. I guess my whole point is that I find some solace in the theme of the movie, which Chuck Noland states near the end as he tries to come to grips with the new reality he faces when he returns home and says:
“And I know what I have to do now. I gotta keep breathing. Because tomorrow the sun will rise. Who knows what the tide could bring?”
We are holding out hope that the tide will bring in something good for Drew, and in the meantime, we have to remind ourselves to keep breathing as well.