The Chronic Phase: Trying to Get Some Traction
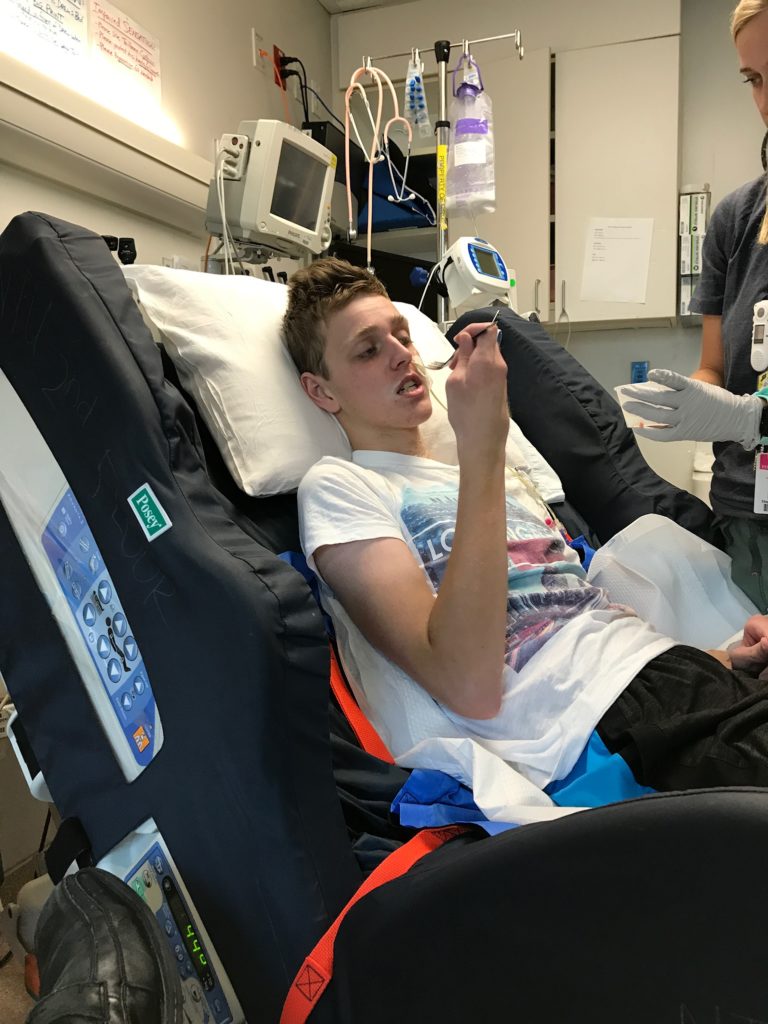
The Social Worker at Primary Children’s Hospital told us that writing in a journal can be therapeutic. Even more, perhaps sharing our journey these past few weeks may help other families with children who suffer from this rare, devastating syndrome (F.I.R.E.S. = Febrile Infection-Related Epileptic Syndrome) or other chronic conditions.
Rehab Team, Day #9 (Saturday, September 16th)
79 days since onset.
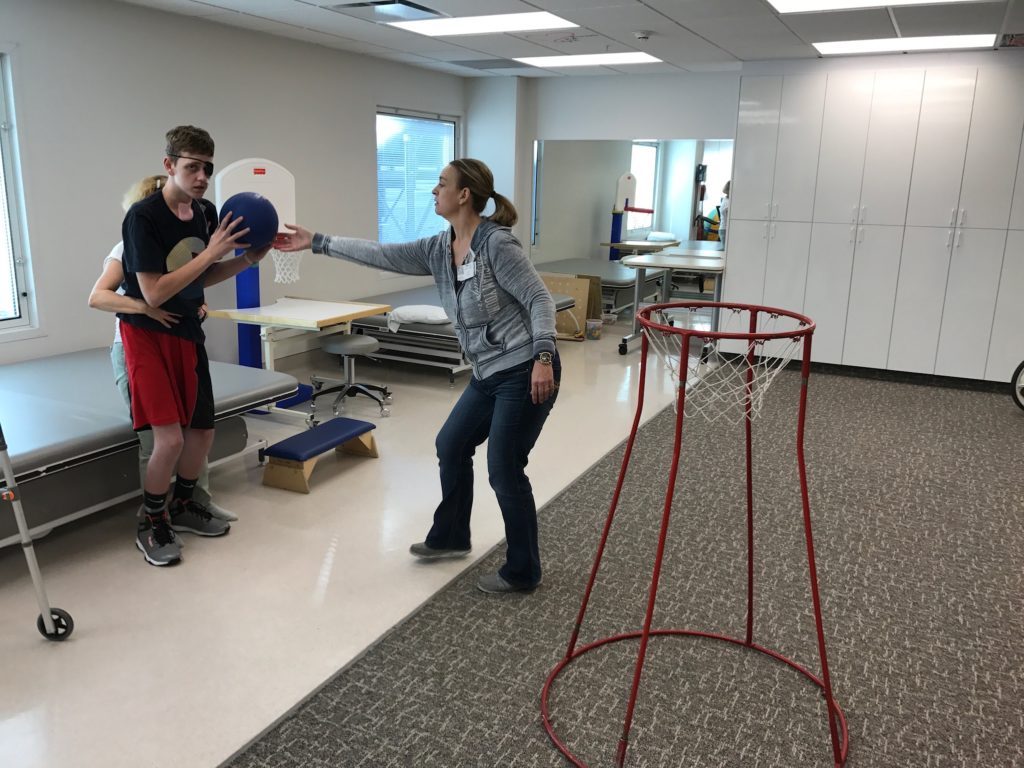
7:00 PM: Drew had a pretty decent day riding the bicycle and shooting a small basketball for physical therapy. He sorted his clean laundry and folded his clothes with occupational therapy. He practiced memory and word-recognition games with speech therapy. Then in the afternoon, Drew was able to watch a little bit of the BYU versus Wisconsin football game before falling asleep (the game was ugly anyway) for a 90-minute nap.
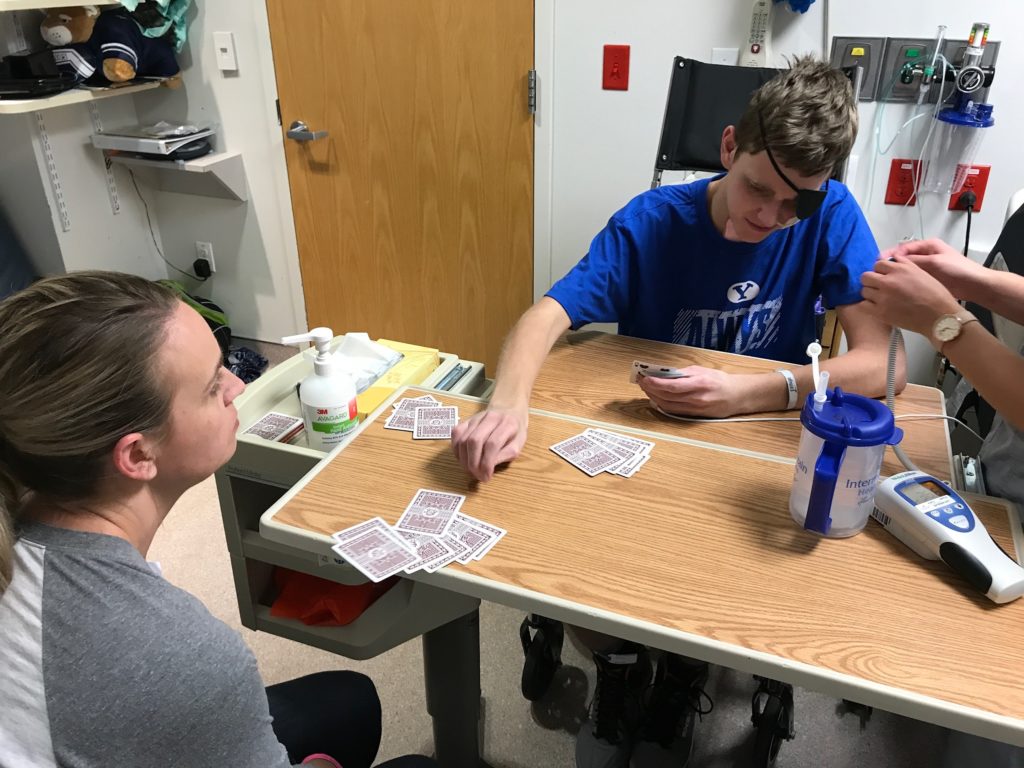
He had a really good evening playing cards (War and Go Fish) with his family, especially once they brought him an eye patch. We were noticing the last several days that as Drew would try to read or look at his phone, he would close his left eye and look through his right eye. As the therapists would work with him, he would constantly say that his right eye was clear and worked well, but the left eye seemed blurry and was not lining up with the right eye. As we put the patch over his left eye, he had a much easier time looking at his cards and playing the games tonight. There are plans for an Opthamology consult later in the week.
9:30 PM: Drew starts getting ready for bed by 8:30 most nights because he gets a bunch of seizure medicines at about 8:15, and when they start to kick in 20 to 30 minutes later, he pretty much falls asleep even if he is in the middle of playing cards. So we try to get teeth brushed and ready for bed just after his medicines are given.
Drew had been in bed and falling asleep as the nurses were doing vital signs and performing their shift assessment tonight, but they had to re-dress the bandage covering the bedsore on his tailbone. As he seemed to already be asleep, the nurse’s aide helped roll Drew onto his side and held him there while the nurse worked on the bandage. However, Drew woke up and flew into a rage.
“Will you stop bullying me?” Drew yelled at the nurse’s aide who was helping to roll him. He pushed hard against the bed rail and fought with the nurses to roll away from them.
”Why are you doing this to me?” He said as he glared at the aide.
The nurse said, “Drew, we need to change your bandage on your back — can you roll over for me?”
”Leave me alone,” Drew yelled as he took a swing at the nurse and tried to hit her. He then tried to punch the nurse’s aide in front of him.
Dawn and I then jumped up and went over to the side of Drew’s bed. His mother tried to calm him down and remind him where he was while I held his hands to stop him swinging at the nurses. It took all of us working together to finally help him to relax and turn for the nurses. Unfortunately, his bed sore has “stalled” according to the Wound Nurse, and we are trying some different bandages and a medicine called Meta-honey to see if it can help the wound to heal. The bed sore is about the size of a small matchbox and goes about halfway to the bone, which is better than it was in the ICU, but hasn’t changed for a couple of weeks now.
This is the third Saturday night in a row that I was able to go home and sleep in my bed. Drew’s older sister has volunteered to come up from school on the weekends and stay with Drew on Saturday nights so that I can go home and get some sleep and get to all of my church meetings more easily on Sunday mornings.
Rehab Team, Day #10 (Sunday, Septemer 17th)
80 days since onset.
4:10 AM: The bed alarm went off as Drew tried to climb out of bed. However, as soon as his sister stood up, he remembered he was in the hospital and stopped, and then he went back to sleep for a while.
11:30 AM: He had a good breakfast and got dressed once his mother arrived at the hospital. He fell asleep just before church was to start at 10:30, so they missed the meeting. But the church leaders came around after the meeting and offered the sacrament in Drew’s room. The leaders blessed the sacramental emblems and then gave them to Drew, his mother, and his sister.
Later when I arrived at the hospital, Drew said, “Hey, Dad! Guess what?”
“What?”
“When they blessed the sacrament in my room, they said to ‘bless the bread and this piece of cheese….” He paused for a moment to look at me and see if I understood.
“No they didn’t, Drew,” his mother corrected.
He seemed serious and intense, but then the corners of his mouth slowly turned upward and Drew started chuckling.
She explained to me that they do have to give him a piece of cheese instead of bread because of his Ketogenic diet, but they didn’t change the words of the prayer. Sometimes it is hard to tell if Drew is joking or not, but once he started giggling at his joke, we all started laughing.
5:30 PM: Drew fell asleep not long after I got to the hospital. He typically has a rest break in the morning and another one in the afternoon, not necessarily to sleep, but just to give his healing brain a rest from any stimulation. We turn the lights out and keep the room quiet, so he usually falls asleep anyway, but we were told to limit his naps to 60-minutes, if possible.
This afternoon, we started to wake him up from his nap so that he could visit with some family and cousins who had come up to the hospital. However, he was struggling to wake up. We try tickling him, pinching his legs (softly), and sometimes even ice packs. He woke up enough to get up to his wheelchair, but then fell back asleep while we moved to the lobby.
Because his room is relatively small, and to minimize noise and overstimulation, the doctors had limited Drew to no more than 2 visitors at a time in his room. So today, we thought we would go down to the lobby where there was more room for everyone. There would still be a lot of noise, but it wouldn’t be as confined.
Once in the lobby, we woke him up again, and then he was able to visit with some of his cousins he hadn’t seen since before he got sick. After a few minutes, he recognized them and gave them hugs. Even though he kept mixing up their names, he actually remembered them and had a nice visit. As he gets tired or over-stimulated, he will perseverate or forget words, and he has a harder time hearing and understanding what is said to him. We try to speak loudly and stand in front of him when we talk to him, and that helps him to understand. His grandparents and his aunt and uncle were also there. A short time later, three of his friends from school came and they visited quite a while with Drew before and after dinner.
Rehab Team, Day #11 (Monday, September 18th)
81 days since onset.
1:30 AM: I awoke to the sound of Drew’s bed alarm. I opened my eyes and saw Drew’s legs hanging over the bed rail.
”Drew, stop,” I yelled. “Where are you going?” I jumped up and ran over to stop him from getting out of bed. The nurse ran into the room as I grabbed Drew’s legs and pushed them back over the rail.
”Dad, I need to get up and brush my teeth,” Drew said, and then he tried to squirm out of my grip and swing his legs again.
”No, Drew,” I said. “It’s the middle of the night still.”
”We’ll brush your teeth in the morning,” the nurse said as she worked to reset the bed alarm.
”Where’s my phone?” Drew asked. I handed his phone to him. He pushed the button to illuminate the screen, and then he squinted and read the time. “One-thirty,” he read aloud.
”Yes,” I said. “In the morning. You need to go back to sleep until 7:30.”
”OK,” he said as he closed his eyes and pulled his blanket up to his chin. It took a few more minutes, but he finally drifted back to sleep. Once I was sure he was out, I slowly retreated to the fold-out couch and laid back down.
4:30 AM: He woke up again, but this time he didn’t yell or try to get out of bed. I could hear him fidgeting in the bed, so I opened my eyes and saw that he had grabbed the bedrail with both hands and had pulled himself up so that he could peek over the padded bedrail.
I didn’t say anything, but I waved at him. He waved back.
”It’s still the middle of the night, Drew. You need to get some more sleep.” Without a word, he rolled back into the bed and closed his eyes. I watched for several minutes to make sure he wasn’t playing possum and attempting another bed exit, but I could hear his snoring start back up again and I knew he was asleep.
7:30 AM: Drew woke up two more times in the night, but once was when the nurses emptied his bladder at 6:00 AM, so it wasn’t entirely his fault. At least he was more easily oriented to remember he was in the hospital and he was able to more quickly fall back asleep.
I had started waking Drew up again so that he can get out of bed and up to his chair for breakfast. He was starting to rouse when the nurses entered the room. The night nurse and day nurse finish up their shift-change report in the room beside the patient’s bed.
As she finished up her report, the night nurse leaned closer to the bed and said, “Drew, I’m going home now.”
“What?” Drew has half-asleep still, and nearly automatically raised both his arms and said, “Well, alright then. Come give me a hug.”
“Well, OK,” the nurse said.
As she leaned forward and Drew wrapped his arms around her shoulders, she said, “Hey, Buddy, you need to brush your teeth — your breath stinks.”
Without missing a beat, Drew responded, “Well, so does yours.” Drew didn’t laugh, but the rest of us did.
8:00 AM: Once Drew was awake and transferred into his chair, I pulled his bedside tray closer and helped put the straw in his breakfast smoothie.
“Dad, I’m sick of shakes.”
”I’m sorry, bud,” I said. “This is all you can have right now. We’ll talk to the doctors later today and see if we can change it.”
“Fine,” he said. However, I encouraged and cued him for the next 20 minutes and he reluctantly took a few swallows. Finally, he pushed the cup away and said, “No, I don’t want any more.”
”Fine,” I said. “I don’t blame you.”
I took the unfinished smoothie back out to the nurses’ station. The nurses have to calculate how many calories he ate, and then they re-start his tube feeds between therapy sessions so that he can still get his nutrition and recommended calorie intake.
4:30 PM: I got off of work a little early, and it is a good thing I did because the Neurology attending doctor came to discuss Drew’s diet and other concerns with us. After much discussion, the Neurology Team had agreed that because his wounds are not healing and he is already getting sick of the diet, they are going to start weaning him off of the diet (just like any medicine, they have to gradually decrease it). The goal is to have him off of the diet before he leaves the hospital, and in a way, it will be nice to have him supervised for any possible increase in his seizures as they wean him off the diet and they can adjust stuff here if they need to. No seizures today, and he had a 2-hour nap through lunch, so he did really well in therapy this afternoon. He rode the bicycle outside again this afternoon, and he played several games with OT.
The Neuro doctor said that with the FIRES kids, they will have some seizures when they go home, but they typically don’t go back into status epilepticus (the non-stop seizures) once they enter the chronic stage. As we adjust his medicines they can go slow and make sure the seizures stay under control now. The rehab doctors were saying that even with the 4.5 to 1 ratio, he is barely staying in ketosis, and with his slow-healing wounds, it only makes sense to wean the diet first instead of waiting 2 to 6 months like they normally would. With that decision, they will change his ratio to 4:1 for this week, 3:1 next week, 2:1 the following week, and then finally have him on a normal diet for about a week or so before he goes home. Hopefully that will also allow time for his bedsore and tracheostomy wound to heal before he leaves the hospital.
Rehab Team, Day #12 (Tuesday, September 19th)
82 days since onset.
9:30 AM: Drew had a better night and only woke up twice, but unfortunately, he had a really hard time waking up for breakfast. Before I left for work, he was also having a hard time staying awake for his PT and OT sessions. In fact, he started falling asleep while putting on his socks, and then again later, he fell asleep while kneeling and working on his balance. I had to leave for work, but Dawn said they barely got him into the wheelchair and returned to his room, and because he was so sleepy, they reclined the wheelchair and let him sleep there until lunch arrived at 11:00.
9:45 PM: I returned a little later tonight after finishing my church meetings and found Drew asleep in bed and Dawn sitting on the couch crying. I held her for a while and let her cry. She finally explained that Drew had a better afternoon and evening, but she was sad after Drew had a visit from his best friend and girlfriend. Drew was asking his best friend all sorts of questions about school and classes, because they were supposed to essentially have the same schedule this semester. As they talked, Dawn said she could tell that Drew was feeling left behind and missing school, and after they left, he was really wanting to get out of the hospital and be back with his friends at school.
”Why did this have to happen?” She asked me. “This isn’t the way his Senior year was supposed to go.”
”I don’t know,” I said. “But at least we still have Drew with us.”
Rehab Team, Day #13 (Wednesday, September 20th)
83 days since onset.
8:00 AM: “Good morning, Drew,” the Nurse Tech said. “Time for your breakfast.”
Drew groggily opened his eyes and looked at the Tech. “Don’t tell me it’s another smoothie,” he said.
“Ok,” the Tech said. “I won’t.”
After a moment, Drew asked, “So, is it another smoothie?”
The Tech smiled. “You’ll have to ask your nurse.”
His nurse walked into the room holding Drew’s breakfast.
Drew couldn’t see what she was holding, so he asked, “Is it another smoothie?”
The nurse, unaware of the previous conversation, shook her head and said, “Yes.”
“Ugh!” Drew said as he closed his eyes and shook his head. “At least I hope it is strawberry.”
As she read the writing on the lid, she smiled and said, “Looks like we at least got that part right — it’s strawberry.”
“Ok, then,” Drew said as he started moving his legs towards the edge of the bed. “I’ll get up. But I can’t believe its another smoothie.”
10:00 AM: Drew struggled to stay awake all through breakfast and his morning therapy sessions. Today he started falling asleep while putting on his socks, and he was barely staying awake while shooting baskets and walking to his room with physical therapy. He had a very hard time just standing up straight, and he leaned heavily on the walker as he walked, nearly falling multiple times if not for the physical therapist pushing and pulling on him to keep him upright. Every step we had to cue him for safety, balance, and direction to his room. When he finally made it to his room, Drew laid down on his bed and immediately fell asleep, which was too bad because he was scheduled for a visit this morning from the Copper Hills High School Principal, Mr. Quarnberg, and Drew’s Counselor, Mrs. Walters. Dawn and I visited with them as Drew slept. They reviewed Drew’s progress towards graduation and allayed our fears about him missing so much school. They assured us that they will work with the hospital Education Specialist to track his work while he is here, and then once he returns home, we will work with the school and his doctors on his gradual return to school. As a very nice gesture, they brought him a school blanket, and encouraged him that lots of people and peers are praying and hoping for his recovery and return.
8:00 PM: Better afternoon, but little progress. Drew had a 90-minute nap through lunchtime and missed lunch, and then after his afternoon therapy sessions, he fell asleep again and missed Music Therapy. The one bright spot was his evening shower. He finally seemed alert and awake, and he walked with the walker and a lot of assist down to the shower room at the far end of the unit. He tried to do as much of his shower as possible, although with his tracheostomy still open, I had to sit and keep the bandage covered and dry as much as possible.
Rehab Team, Day #14 (Thursday, September 21st)
84 days since onset.
8:30 AM: Instead of hollering my name the last couple of nights when he wakes up, he will lift his head up and look for me on the couch on the opposite side of the room. Or he will grasp the bedrails with both hands and pull himself up to look for me. I still wake up when I hear him moving in bed, so I wave at him to let him know I see him, and then he waves back. I haven’t had to remind him as much that he is in the hospital, but I do have to remind him that it is still the middle of the night and he needs to go back to sleep. The last several nights we were relying on Trazadone to help him stay asleep, but we finally realized that in combination with all of his other seizure medicines, the minimal dose of the sleeping medicine was amplified by the sedating effects of the rest of his medicine, so he was struggling to wake up in the morning, and struggling even more to stay awake the last few days. So we discussed with the doctors, and last night was the first night without any sleeping medicines and it seemed to make a big difference.
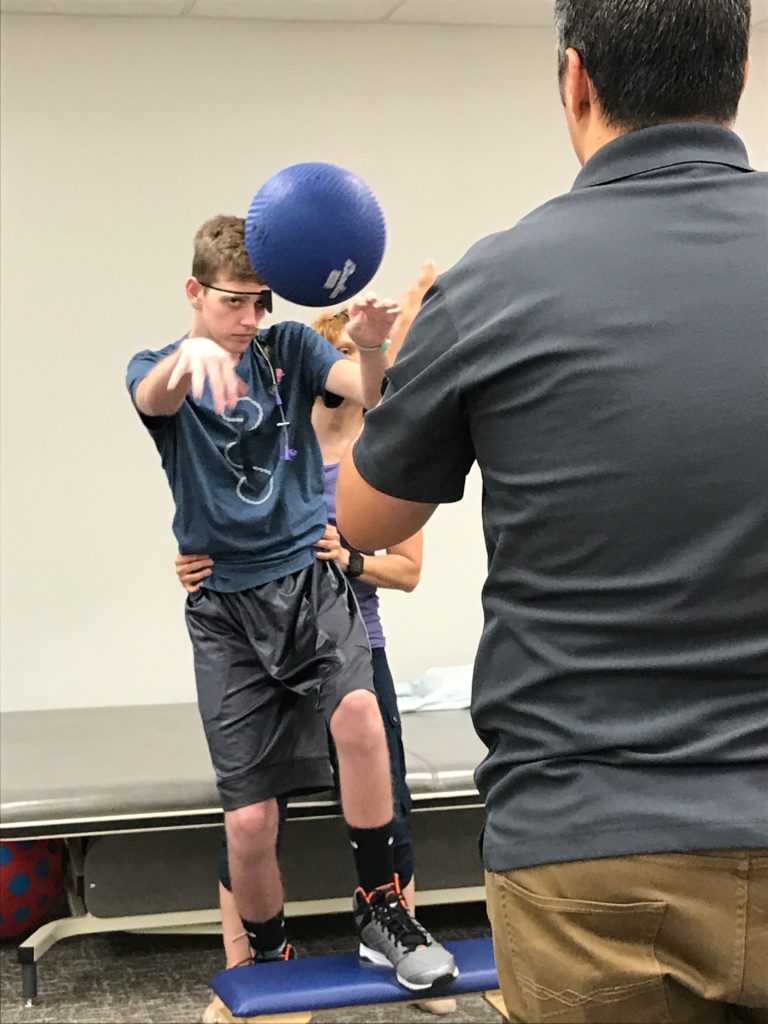
Finally a day where we felt like we weren’t just spinning our wheels. He practiced getting dressed with OT and he put his socks on nearly independently. With physical therapy, he walked all the way to the Rehab Gym with a walker (still lots of assistance and verbal cues). Once in the gym, he played Uno with the therapist and his mother while he practiced unsupported sitting, reaching, and holding his cards. In the afternoon, he went for another bicycle ride with physical therapy, along with more practice walking. Finally with Speech Therapy he played memory games with cards and worked on word-finding as he still struggles to remember names of items, or he calls them the wrong word (which is similar to his very first symptoms of being sick, before the seizures even started).
He finished the day with a visit from his brother, Alex, and his brother’s friend. They played WAR, and even though he lost the card game, he was actually somewhat civil in defeat and not so competitive for a change. While his brother was here, we also walked to the end of the hallway and back, touched the ceiling, and had him stand next to his brother to see how tall he was in comparison. The only problem is that Drew kept trying to run and nearly lost his balance multiple times. He is still extremely impulsive and very much lacks any safety awareness. Finally a good day all the way around with therapy, rest, and a little more improvement.
Rehab Team, Day #15 (Friday, September 22nd)
85 days since onset.
3:30 PM: I returned to the hospital from work to find Drew in his room working with Speech Therapy, and he hollered, “I don’t like your freakin’ beard or your freakin’ moustache.”
Dawn had stepped into the hallway to visit with one of our neighbors, so Drew had been alone in his room working unsupervised, and he was really acting up today.
“I think you should cut it all off, your freakin’ beard,” Drew said again.
The poor speech therapist was trying hard to redirect Drew to the task they were working on at hand, which was following verbal directions to draw a picture, but Drew was struggling to focus.
“Drew, Drew,” I said as I stuck my face right in front of his, and with our noses nearly touching, I said, “You need to be nice. Stop being so rude.”
”It’s his beard,” Drew said matter-of-factly.
”It’s OK,” the Speech Therapist said. “Drew, let’s try something different.” He then proceeded to pull out the picture cards.
As good as Drew’s day was yesterday, and even with a decent night sleep, he seems to have taken a step backward as far as his behaviors and cognition. He has said lots of rude things to the staff today and isn’t listening when they ask him to help do things, like roll on his side. Fortunately, the nurses and therapists know this is part of the process, but these behaviors can sure try our patience.
4:30 PM: The eye doctor just finished examining Drew. He is from the Opthamology Neurology Team and also video recorded Drew’s eye movements to add to his chart. Essentially, the doctor said there is not much we can do right now to fix his eyes but simply to continue wearing a patch over one eye. His eyes both seem to do well individually, but they are not coordinated together with their movement or focus. The doctor said the way to fix it is to address whatever is causing the vision problems, and at this point, Drew’s vision problems could be due to his brain illness, his prolonged seizures, or three of his seizure medications. Unfortunately, it is too early to say for sure, so in the meantime, wear an eye patch and then we will return to the clinic a few weeks after we leave the hospital.
8:30 PM: “Why are you nurses always reporting what I say?” Drew’s continues to be rude and defiant to the nurses. Not sure if it is official, but in a way, it seems like Drew’s brain is healing similarly to his body. After being so sick and in a come for so long, he needs to re-learn how to roll and sit up and stand and eventually walk and run. In a way, it seems his behaviors and cognition likewise have to progress again through the different stages and phases of growing up. For the past couple of days, he is acting a lot like he is in 4th or 5th grade again. Hopefully this will be a short phase and he will continue to progress to more age-appropriate behaviors, but he may or may not — we just don’t know how much lasting damage was caused by his illness and seizures.
He walked to the shower room again with a walker, assistance, and lots of verbal cues. After, he put a small puzzle together with his sister. It is interesting to note that he still has not regained normal sensation throughout his body. As we were transferring onto the shower bench tonight, he scraped his arm on the doorway pretty hard, but he didn’t even flinch. He cannot feel his feet very well, nor can he tell if he has a full bladder or not, and his balance and proprioception are horrible. The physical therapist today, though, hadn’t worked with Drew in nearly a week, and he couldn’t believe his progress with some things, such as his sitting balance and standing up. Of course, he still has some things to work on and improve in the next 3 or 4 weeks of rehab (vision, sensation, balance, diet, wounds, safety, strength, bladder, cognition, etc.), but hopefully we can continue to make some progress with his physical, mental, and social recovery before he comes home.
The last bit of news we received this afternoon from the doctors was that they agreed to allow us to have a Ride Pass for this weekend, which means we are allowed to take him out of the hospital for a few hours to practice different transfers and activities. We try to achieve a few goals with the outing while also identifying the areas we need to continue to practice for the next 3 or so weeks in Rehab. In order to be ready for anything that might arise, his mother and I were trained how to administer his rescue medicine in case he has a prolonged seizure. We are also getting trained on how to empty his bladder even though we are planning to return to the hospital before he would need to have the straight catheter again. They pretty much said we could take him anywhere but our home, because he would not only be really confused, but it could be very difficult to get him to go back to the hospital. So, we’ll practice and train and see if we can take a field trip on Sunday for a few hours.